June 4, 2025
Ovulation is one of the most important — yet often misunderstood — parts of the menstrual cycle. Whether you’re trying to conceive, avoiding pregnancy, or simply curious about your body, understanding what happens during it, and its symptoms can help you feel more in tune with your cycle and reproductive health.
This guide explains how to recognize when you’re fertile, track your cycle using calculators and test kits, and understand symptoms like bloating, breast pain, backaches, mood swings, and nausea.
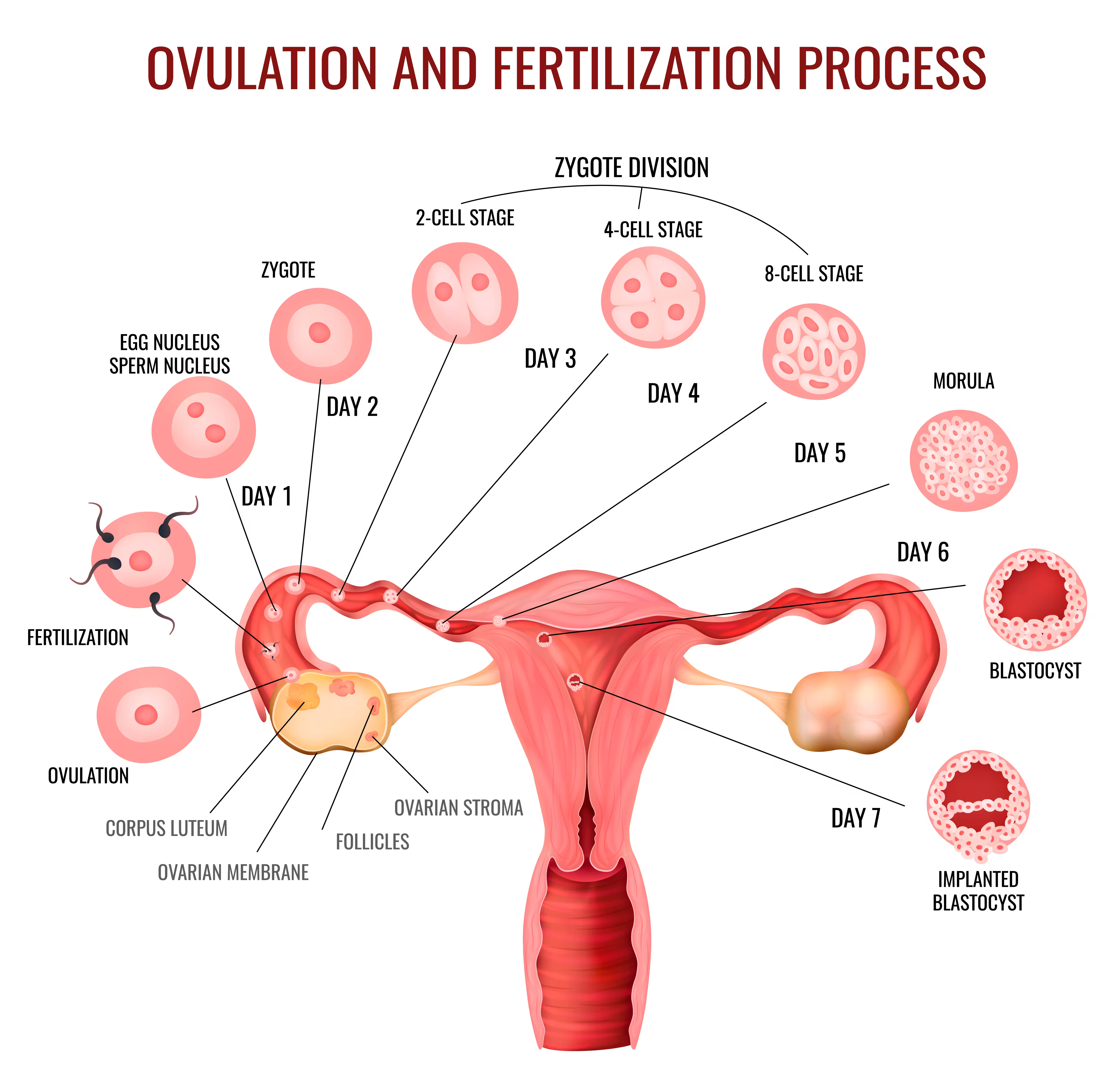
It is the process by which a mature egg is released from one of your ovaries. This egg travels down the fallopian tube, where it can be fertilized by sperm.
This release typically happens once per cycle — around the middle of your cycle — and is triggered by a rise in luteinizing hormone (LH).
Everyone’s body is different, and cycles can vary month to month, so tracking ovulation is key.
| Cycle | Day of Ovulation |
| 28-day cycle | Day 14 |
| 26-day cycle | Day 12 |
| 30-day cycle | Day 16 |
It is the moment your body prepares for the possibility of pregnancy, releasing an egg and creating the ideal conditions for fertilization.
1. The Brain Signals the Start
The process begins in your brain, specifically in the hypothalamus, which releases gonadotropin-releasing hormone (GnRH). This hormone triggers your pituitary gland (a tiny gland at the base of your brain) to release two more key hormones:
2. The Follicles Begin to Grow
In the first half of your menstrual cycle — called the follicular phase — several follicles in your ovaries start to grow due to the rise in FSH. But usually, only one of these follicles becomes dominant. This “winner” follicle nurtures and grows a single egg to full maturity.
As the follicle develops, it produces increasing amounts of estrogen, which helps thicken the uterine lining (endometrium), preparing it for a potential pregnancy.
3. LH Surge Triggers
Once estrogen levels peak, they send a signal to your brain to release a large amount of Luteinizing Hormone (LH) known as the “LH surge”. This surge is what triggers ovulation, the mature egg bursts out of the follicle and is released from the ovary.
This usually happens around the midpoint of your menstrual cycle — for example, on day 14 of a 28-day cycle — although it can vary based on your personal cycle length.
4. The Egg Travels Down the Fallopian Tube
After release, the egg is swept into the nearby Fallopian tube. This is where fertilization may occur if sperm is present. The egg remains viable for about 12 to 24 hours — a short window when it can be fertilized.
5. The Corpus Luteum Forms
Back at the ovary, the empty follicle transforms into a structure called the corpus luteum which begins secreting progesterone, a hormone that helps maintain the thickened uterine lining in case of pregnancy.
If fertilization happens, the embryo will eventually implant into this lining. If not, the corpus luteum breaks down after about 10–14 days, progesterone levels drop, and the uterine lining is shed during your period.
It is a quick event — the egg lives for about 12 to 24 hours after release. But your fertile window is broader than that. Sperm can survive in the body for up to five days, so your chances of conceiving are highest during the five days leading up to and the day of ovulation.
Here are the 8 most common symptoms and signs:
1. Discharge (Cervical Mucus Changes)
You might notice clear, stretchy mucus — often compared to egg whites. This type of discharge helps sperm travel and survive.
2. Cramps “Mittelschmerz Pain”
Many women feel a sharp or dull ache on one side of their lower abdomen. It’s usually nothing to worry about but it can be surprising if you’re not expecting it.
3. Breast Pain or Tenderness
Due to hormonal shifts, some women experience breast pain, similar to what happens before your period.
4. Mood Swings or Emotional Crying
It can affect mood, libido, and even emotions. If you find yourself crying easily or feeling extra emotional, your hormones might be the reason.
5. Joint Pain
Although not frequently discussed, some women experience joint pain due to hormonal fluctuations as estrogen tends to have an anti-inflammatory effect, but its levels dip right before it. This dip may increase joint sensitivity or inflammation, especially if you’re already prone to joint issues or have an autoimmune condition.
6. Bloating and Back Pain
Bloating is a lesser-known symptom, as is lower back pain, but both are quite common.
7. Increased Libido
Your body naturally boosts sex drive during your fertile window — nature’s way of helping conception along.
8. Headache, Nausea, and Night Sweats
Though not as common, some women report headaches, mild nausea, and even night sweats around the time of ovulation.
Not everyone has a textbook 28-day cycle, and that’s where calculators and apps come in handy. These tools use your last period date and average cycle length to predict your ovulation days.
For more accurate tracking, many women turn to:
It’s possible to ovulate and not get your period. If this happens, there are a few common reasons behind it, and not all of them are cause for concern.
1. You Could Be Pregnant
It’s the most likely reason.
If an egg is released and then fertilized by sperm, your body shifts into baby-growing mode. That means your period doesn’t show up. Instead, your body starts producing a hormone called hCG, which is tested by pregnancy tests.
If your period is late and you think pregnancy is possible, take a home pregnancy test—ideally around 14 days after you think you ovulated.
2. Your Period Might Just Be Late
Life throws off our cycles more often than we realize. Even if you did ovulate, your period could be delayed due to:
Your body might just be taking a little longer to start your period. Sometimes the second half of your cycle runs longer than usual.
3. Hormones Might Be Out of Balance
In some cases, you might ovulate but still skip your period because of a hormone imbalance or a medical condition. Some examples include:
4. Others:
In most cases, a single miscarriage doesn’t negatively affect your ability to ovulate or get pregnant again.
However, if miscarriages are recurrent (two or more), it might signal an underlying issue, like hormonal imbalances, disorders, uterine abnormalities, or autoimmune factors. That’s when your doctor might suggest a deeper evaluation, possibly including:
| Treatment | What It Is | Who It’s For | How It Works |
|---|---|---|---|
| Induction | A fertility treatment using oral or injectable medications to stimulate the ovaries to release eggs | – Women with irregular periods – Anovulation (not ovulating) – PCOS – Undergoing IVF | Medications encourage the ovaries to grow and release one or more mature eggs during the cycle |
| FSH Injections | Follicle Stimulating Hormone shots are used to help develop multiple follicles | – Women undergoing IVF or IUI – Women not responding to oral meds alone | Stimulates the ovaries to grow more than one egg, increasing the chances of successful fertilization |
| HCG Injection (Trigger) | Human Chorionic Gonadotropin shot that mimics the body’s natural LH surge | – Used after follicles mature, to time ovulation with precision | Triggers egg release typically within 36 hours, ideal for timing intercourse, IUI, or egg retrieval in IVF |
Hormonal birth control works by preventing egg release, so if you’re on it, you won’t have the typical symptoms. However, once you stop, it may take a few cycles for regular ovulation to return.
| Type of Birth Control | How It Affects Ovulation |
|---|---|
| Birth Control Pills (Combined) | Contains estrogen and progestin, which prevent the pituitary gland from releasing hormones that trigger egg release |
| Progestin-only Pill (Mini-pill) | It may not fully stop ovulation, but thickens cervical mucus and thins the uterine lining to prevent pregnancy. |
| Birth Control Patch or Ring | It works like a pill, releasing hormones that prevent the egg from being released. |
| Hormonal IUD (e.g., Mirena) | Mostly prevents fertilization by thickening cervical mucus; may suppress it in some users. |
| Implants (e.g., Nexplanon) | Releases progestin, which often stops it completely for several years. |
| Birth Control Shot (e.g., Depo-Provera) | Stops ovulation entirely in most women by suppressing hormone release. |
The entire ovulation cycle is regulated by a complex hormone interplay, including FSH, LH, estrogen, and progesterone. These hormones govern everything from egg maturation to the release and eventual shedding of the uterine lining.
If your cycles are erratic or you’re not seeing any signs of ovulation, it could be a sign of:
Talk to your doctor about ways to regulate your cycle and encourage healthy ovulation.
Missing one period now and then isn’t usually a big deal. But it’s a good idea to talk to your gynecologist if:
Whether you’re actively trying to conceive or just curious about your health, understanding what is ovulation, how to recognize signs of ovulation, and when your ovulation fertile window occurs puts you in control.
Use tools like an ovulation calculator, ovulation test kits, and charting apps to get to know your cycle better. Pay attention to symptoms like ovulation cramps, mood swings, or discharge, and don’t hesitate to reach out to a healthcare provider if something feels off.
Ovulation is a powerful signal of your body’s rhythm and health. With knowledge, tracking, and support, you can align with it, whether your goal is pregnancy, cycle awareness, or hormonal balance.
Reference: Emirates OBGYN